
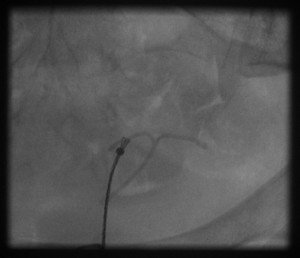
Left image, top panel: Scout frontal radiograph of the pelvis showing the T-shaped contraceptive device before retrieval.
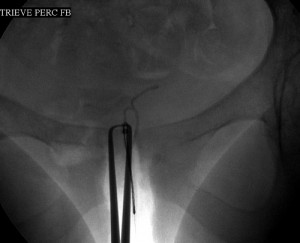
Right image, top panel: The right arm of IUCD is snared and being pulled out
Bottom image: The IUCD is pulled out and lies between the patient’s upper thighs.
Intrauterine contraceptive devices (IUCDs) work best when positioned well in the uterine fundus, no when completely expelled from the uterus, displaced from the uterine fundus, embedded into the endometrium or myometrium, or partially or completely perforate the uterus. Well-positioned IUCDs prevent pregnancy in 98% to 99% of subjects.
IUCD expulsion occurs in 10% of patients and requires replcement with a new one. Displacement of IUCDs is commoner than IUCD expulsion, occuring in 25% of IUCD recepients. It may or may not be symptomatic depending on the location of the displaced device but may be associated with ectopic pregnancy. When symptomatic or if the patient desires, the IUCD should be replaced. IUCD perforating the uterus is uncommon, occuring in 1 of every 1000 women (0.1%) and depends on the skill of the operator, the presence of uterine abnormalities, and low estrogen levels in the patient. It is commoner in women breastfeeding their infants and when IUCD is placed withing 6 months of parturition. When the IUCD penetrates deep into the uterine substance but does not violate its serosa, it is called embeddment and its management varies, requiring at a minimum empiric antibiotic treatment and an attempt at removal of the IUCD. But full-thickness uterine perforation is a more serious situation, with the IUCD either completely or partially within the peritoneal cavity. The most common sequela of partial uterine perfoation by an IUCD is omental adhesion, whereas its complete intraperitoneal expulsion may be asymptomatic or cause peritonitis, sepsis, fistulas, or bowel obstruction or perforation.
Usually IUCDs are removed in a physician’s office at the patient’s request, or when the IUCD’s effectiveness lapses, or when it causes problems, or when a complication occurs. To do so requires visualization of the string attached to the base of the IUCD stem at the external cervical os and grabbing it with a pair of alligator forceps or an IUCD hook. Whenoccasionally the string is missing at the cerical os, the IUCD may be removed with a hysteroscope or ultrasound gauidance or it may be snared and removed under fluoroscopic guidance as in this patient, who was referred to the interventional radiology clinic by a gynecologist.
She was brought to the interventional radiology procedure room at a hospital and while in semi-lithotomy position and under asceptic conditions and antibiotic coverage, I performed cervical anesthetic block. With a pair of tenaculum forceps helping to straighten her cervical canal, I passed an EnSnare device into her uterine cavity. Because the base of the IUCD stem was elusive, I snared its right arm and removed it from the patient without complications. She was observed briefly at interventional radiology holding area and went home without problems. She did well afterwards.



