What are percutaneous vertebroplasty & kyphoplasty?
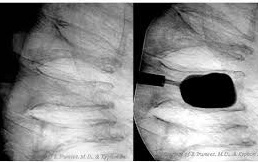
Vertebroplasty is restoring strength to a fractured vertebra (backbone) by injecting a chemical (bone cement) into it through a hollow tube introduced into the bone from the back. The chemical permeates the lacelike spaces in the bone including the fracture planes, hardens, and reinforces it.
Vertebroplasty
Kyphoplasty
Kyphoplasty is the repair of a hunched back caused by compressed vertebral fracture(s). It is typically achieved by inflating a balloon inserted into the crushed vertebra through in- struments advanced into it from the back. The inflation creates a cavity or space into which bone cement is injected. Thus, not only is the bone stronger, it is ‘taller’ and the back hunch-free. Both procedures are commonly done under cover of conscious sedation (light sedation) and local anesthesia, allowing patients to go home the same day.
What are the indications for vertebroplasty and kyphoplasty?
Osteoporosis

Multiple myeloma
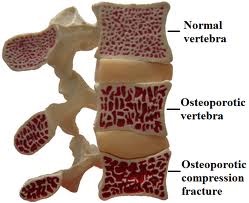
The typical patient is one who broke their backbone(s) in a fall or, who through some other means damaged a backbone and whose pain does not respond to adequate pain medication, physical therapy and back braces. Osteoporotic vertebral fractures take 4 weeks to 12 weeks to heal and can be a source of constant back pain and altered lifestyle. Over 80% of people with such painful fractures are pain-free after vertebroplasty or ky- phoplasty. The re-enforced bone remains fit and painfree until another fracture occurs at another level of the spinal column.
Who is at risk for vertebral compression fractures?
People at risk for fractures of the backbone include those with osteoporosis or other medical conditions that weaken the bone, such as multiple myeloma (MM), vertebral hemangioma or metastatic cancer. By far the commonest of thses is osteoporosis, which is commoner in elderly Caucasian females. In this non-malignant condition the amount of calcium in bones is low, placing them at risk for fractures with little or no stress or provocation.
How do I know I need vertebroplasty or kyphoplasty?
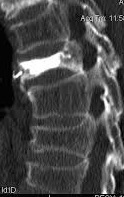
If you are an elderly person or someone with any of the conditions referred to above that weaken bones and you have back pain with or without a fall that has not responded to conservative measures, you may wish to see your healthcare provider. Plain x-rays, CT scan, or MRI of your back will help determine if you need to see a specialist such Osteoporosis Multiple myeloma as an interventional radiologist for vertebroplasty or kyphoplasty. People with healed vertebral fractures are unlikely to benefit from these treatments. In such persons, oth- er causes of back pain should be sought. It is for this reason that most practitioners of vertebroplasty and kyphoplasty rely on MRI of the spine to determine if a suspected vertebral fracture is responsible for a patient’s back pain, in addition to it being able to uncover unsuspected reason(s) for such pain.



