History
A 39-year-old parous woman presented to an emergency department with lower abdominal pain and CT scan of her abdomen was obtained as part of her investigation. Although the examination revealed no acute explanations for her symptom, it showed that her gonadal and pelvic veins were dilated, an observation present on a CT scan of her abdomen and pelvis obtained 3 years earlier. She was later referred to an interventional radiology clinic (IRC) for consultation for pelvic congestion syndrome and possible gonadal vein embolization. Her medical history revealed a 6-year account of chronic abdominal pain, heavy menstrual periods, dysmenorrhrea and ultrasound-proven uterine fibroids. She had no gastrointestinal complaints except for diverticulosis without diverticulitis, nor did she have urological complaints or other gynecologic problems. There was no investigation of her psychological past nor were there any obvious manifeststions of its perturbation. She later had a pelvic MRI that did not confirm her past report of uterine fibroids but confirmed pelvic varices and bilateral gonadal vein dilation.
She first underwent bilateral ovarian vein embolization with improvement in her symptoms that significantly improved after she underwent staged bilateral pelvic vein embolization several weeks later. She continues to do well and is still being followed at the IRC.
Radiologic findings
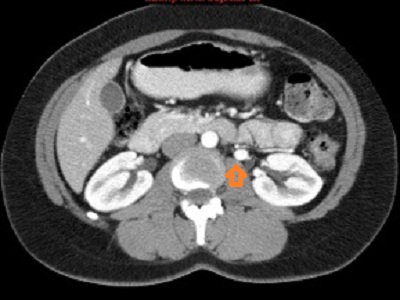
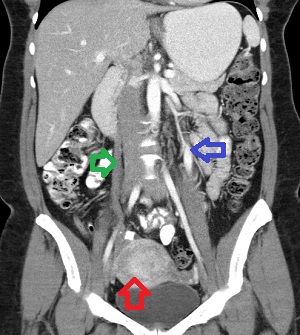
First row, left to right: Axial (1st image) and coronal (2nd and 3rd images) contrast-enhanced MDCT scan of the abdomen and pelvis showing contrast opacification of the left ovarian vein in the arterial phase of the study (orange arrow on the 1st image and blue arrow on the second image) and unopacified but dilated right ovarian vein (green arrow on the 2nd image). There is beginning opacification of varicose uterine plexus arrowed red on the 3rd image.
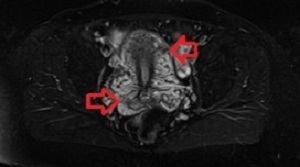
Second row, left to right: Axial fat-suppressed T1WI of the pelvis of the same patient demonstrating dilated and tortuous uetrine and vaginal venous plexuses
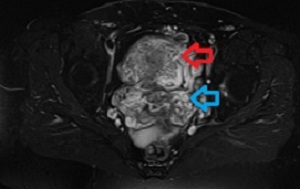
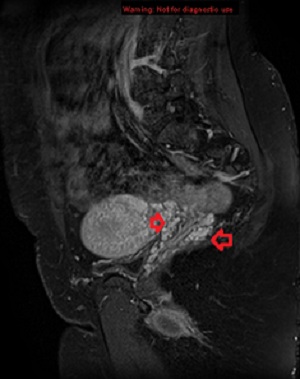
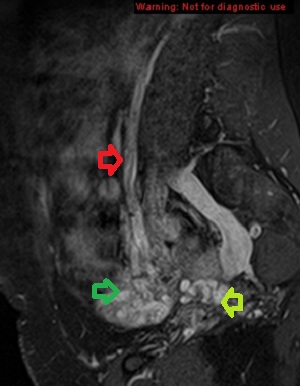
Third row, left to right: Saggital fat-suppressed T1WI of the pelvis showing on the left image dilated left vaginal plexus and, on the right, dilated left ovarian vein (red arrow), dilated left ovarian plexus (blue arrow) and dilated pelvic veins (yellow).
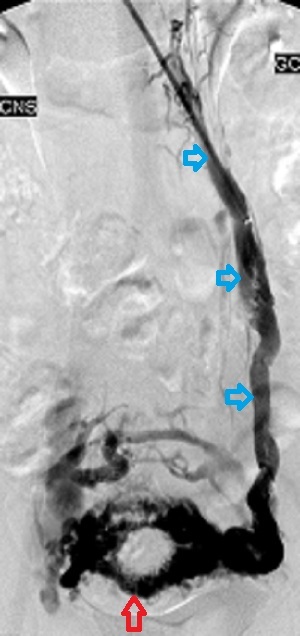
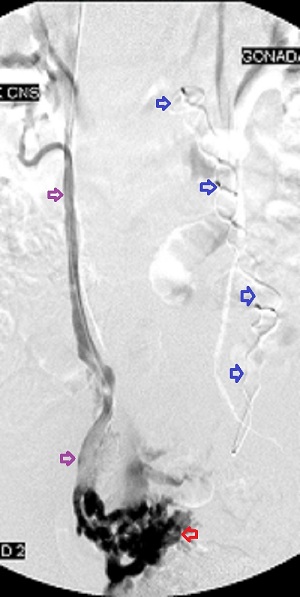
Fourth row, left to right: First image, selective catheter left ovarian venogram showing dilated left ovarian vein (blue arrows), crossfilling of the contralateral pelvic veins through the uterine arcuate branches (red arrow). Second image, selective right ovarian venogram after embolization of the left ovarian vein confirming dilation of the vein (red arrows) and showing no opacification of the left pelvic veins across the uterine arcuates, proving successful embolization of the left ovarian vein (blue arrows). Third image, right and left ovarian veins after their embolization during right internal iliac venography.
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
Discussion
Chronic pelvic pain in premenopausal women is common, being the reason for 10% of outpatient gynecologic visits. It is a symptom of several disorders that span multiple organ systems including gynecologic ( leiomyomas, endometriosis, adenomyosis, ovarian and tubal disorders, pelvic inflammatory disease), gastrointestinal (irritable bowel syndrome, inflammatory bowel disease) and urologic disorders. It is also a psychologic complaint in 40% to 60% of women with documented history of childhood sexual abuse and may be a somatization disorder. But when such pain occurs in a premenopausal woman, especially if multiparous, for 6 months or more in the presence of dilated ovarian or pelvic veins and has no explainable reason, it meets the definition of pelvic congestion syndrome (PCS). Thus, PCS is a disease of exclusion that requires multidisciplinary approach. The pain in pelvic congestion syndrome can be nonspecific, may occur with sexual intercourse, or PCS may manifest as persistent genital arousal or urinary urgency. The pain may be premenstrual, menstrual, or perineal and is aggravated by acts or states that raise the intra-abdominal pressure such as bending, lifting, defecation, and prolonged standing or walking. PCS is often associated with vulvar, perineal, and lower extremity varices as well as polycystic ovaries, the number and sizes of the ovarian cysts varying.
The normal ovarian vein measures 3 to 4 mm on catheter venography and drains into the left renal vein on the left, often at a right angle, and frequently directly into the IVC on the right. It begins its journey from the ovarian plexus that lies next to the ovary and which communicates with the uterine plexus within the broad ligament, the latter joining the vaginal plexus to form the uterine vein which drians into the internal iliac vein; the internal iliac vein then joins the external iliac vein to form the common iliac vein, which joins the contralateral vessel to form the IVC. The ovarian vein ascends, anterior to the psoas muscle, to the left renal vein on th left and to the IVC on the right. It has valves that prevent reflux, but autopsy studies have shown these to be absent in the proximal left vein in 15% of subjects and in 6% on the right. Further, the valves are incompetent in 35% to 45% of multiparous women.
The cause of PCS is unclear but presumed multifactorial. But its proximate cause is ovarian or pelvic venous reflux and retrograde flow. Thus it is found in women who lack ovarian valves or whose valves are incompetenct, those with obstruction to ovarian venous flow due to stenosis or occlusion, in the nutcracker syndrome due to compression of the left renal vein between the superior mesenteric artery and the abdominal aorta impairing left renal venous drainage, and women with retro-aortic or circumaortaic left renal veins, inferior vena cava (IVC) reflux, or pelvic masses that distort the iliac veins and impede flow through them. Since it is commoner in multiparous women it is supposed that the 60-fold or so increase in venous traffic through the ovarian and pelvic veins associated with pregnancy may play a role in its causation.
Diagnosing pelvic congestion syndrome is challenging because it shares its principal characteristics with other conditions: though it occurs more frequently in multiparous women, it occurs in nulliparous women, too; on CT, dilated and incompetent ovarian veins in asymptomatic parous women are a frequent observation and do not constitute PCS when seen as isolated findings; chronic pelvic pain, the chief complaint of sufferers of PCS, is caused by many other organic conditions as mentioned above. For these reasons, its disgnosis should begin with a thorough review of a patient’s past medical and psychiatric history and further investigations predicated upon their findings.
The radiologic workup of suspected PCS should begin with grey-scale and color Doppler ultrasonography confirmed with contrast-enhanced CT scan of the abdomen and pelvis, magnetic resonance imaging or selective catheter ovarian and pelvic venography. Trans-abdominal and endovaginal pelvic sonography is cheap, universally available, and quick to perform. On grey-scale imaging it shows dilated (>5 mm) and tortuous pelvic veins with sluggish flow (~ 3 cm/sec) which on color Doppler interrogation augment their flow in the standing position or during Valsalvar maneuver. It also reveals dilated pelvic veins and uterine crossing veins (arcades), the latter strongly predictable of the finding of crossing uterine veins at venography. The demosndtration of reversed flow in the distal left ovarian vein highly correlates with left ovarian valvular incompetence on catheter venography although it can occur in normal subjects. Pelvic sonography also shows ovarian cysts well which can occur in pelvic congestion syndrome. Finally, it is used to monitor embolized ovarian veins. Contrast-enhanced multidetector computed tomography (CE-MDCT) demonstrates ovarian reflux well but is encumbered by the use of radiation and iodinated contrast as well as its inability to show the direction of venous flow. It demonstrates left ovarian vein incompetence and reflux by its opacification (and incompetent right ovarian vein when it anomalously returns to the right renal vein) during the arterial phase of the study, when only arteries and the left renal vein should opacify. CE-MDCT also allows measuremnt of the ovarian and pelvic veins and demonstrates their dilation and tortuosity when present. As in our case, it may allow a view of dilated uterine arcades that predicts cross-filling during catheter venograpy. It shows ovarian vein stenosis, collateral venous branches and the nutcracker phenomenon when present. Like ultrasonography, CE-MDCT can be used to monitor treated varices and like ultrasonography and MRI, it allows panoramic search of the abdomen and pelvis for diseases in other organ system that may cause chronic pelvic pain. Magnetic resonance imaging, preferrably with gadolinium enhancement, should not be the initial modality of investigation of PCS, rather it should be used to answer specific questions raised by sonography or CT imaging of the pelvis during workup for the disease. But since it is increasingly used for the investigation of other abdominal and pelvic disorders, it may provide unexpexted information on the state of ovarian and pelvic veins. Advances in MRI technology allow not only the depiction of ovarian and pelvic venous dilation but also the direction of venous flow that permits portrayal of reversed flow. Current embolic agents used to treat PCS cause artifacts on MRI that prohibit its use to monitor the treatment. The gold-standard for the diagnosis of ovarian vein incompetence and reflux is selective catheter venography on a tilting table. First performed in 1965, it is invasive compared to the cross-sectional imaging modalities and should be reserved for situations when intervention is planned. The procedure can be performed transfemorally or transjugularly (I favor the transjugular route) and involves, first left ovarian venography for the nutcracker syndrome and then selective left and right ovarian venography. A positive study shows dilated ovarian veins ( 8 to 10 mm to account for magnification) with dilated and tortuous ovarian, uterine, and vaginal plexuses, cross-filling of contralateral vessels across the uterine arcades, and dilated pelvic veins.
The management of PCS can be conservative or aggressive. A conservative approach is pursued when a patient choses to do so or in recognition of the fact that not all patients respond well to current active treatments and that some of those who initially respond relapse later. In addition, since the principal complaint of PCS is chronic pelvic pain which may have psychiatric or psychosocial underpinnings, it is frustrating to both the patient and the care giver when symptoms return after treatment. For these reasons it is prudent to fully evaluate a patient for all potential causes of chronic pelvic pain including psychiatric factors and to fully outline the benefits and risks of any purposed interventions as well as their limitations and expectations. It is important to stress the likelihood of relapse that occurs with most venous disorders.
Before the introduction of gonadal and pelvic vein embolizations in 1994, medical therapy in the form of non-steroidal anti-inflammatory drugs, oral contraceptives and gonadotropin releasing hormone agonists and hysterectomy were the treatments of chronic pelvic pain. The use of a multidisciplinary approach addressing somatic, psychological, dietary and other factors was proven more effective than medical treatment. Hysterectomy and bilateral salpingo-oophorectomy for pelvic congestion syndrome in women who had no desire to maintain their fertility was shown in a small study to relieve or improve symptoms in 35 of 36 subjects (97% clinical success rate), however, it has been shown by another study that symptoms persisted in 22% of patients treated with hysterectomy (with or without bilateral salpingo-oophorectomy). By contrast, the technical success rate for ovarian and pelvic vein embolization ranges from 88.9% to 96.7%, while the clinical success rate varies from approximately 58% to 89%. But the treatment is a relatively safe same-day procedure with no limitations on a patients activity that can be offered to women who are yet to complete their family and desire to retain their uterus.
In summary, PCS is a common but frequently overlooked disabling condition in premenopausal women that shares common presentation with several disorders of other organ systems. Its diagnosis is one of exclusion and its management multidisciplinary. Currently, ovarian and pelvic vein embolization for the disease is safe and offers reasonable clinical relief of its symptoms.



