







Diabetic foot ulcers are frequently difficult to treat for a number of reasons: diminished ability of the body to fight infections and heal; polymicrobial colonization of wounds; poor glycemic control; neuropathy and vasculopathy. Vasculopathy occurs at visible and occult levels and is a frequent reason for lost tissue in limbs and ultimately limb amputation. Primary care givers, podiatrists, and vascular specialists are joined in an aggressive campaign against this problem and the tool box of endovascular specialists is ever swelling with new equipment for tackling this problem. These include instruments that remove plaques (atherectomy), those that liquefy clot (thrombolytics), balloons that dilate stenosed vessels, and, of course, stents that prop vessels open once dilated.
In this patient, a 67 year-old woman with long-standing diabetes, there was a plantar ulcer of her anterior left forefoot that resisted healing despite many noninvasive treatments. Her podiatrist referred her to me and her sonographic and angiographic investigations revealed multiple significant stenoses in her distal left superficial femoral artery (LSFA), left popliteal artery, and her anterior tibial artery. Her posterior tibial artery was occluded and her chief path of blood flow to the left foot was her left peroneal artery. Her arterial paths above the distal left SFA were open and she had stage 3 chronic renal insufficiency. Faced with the dilemma of continuing foot infection and potential limb loss and worsening renal insufficiency following exposure to radiocontrast, she put off endovascular revascularization of the arterial narrowings for sometime, finally caving to pressures from her son.
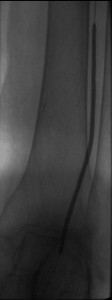
After instituting strategies to minimize contrast-induced nephropathy, I employed atherectomy of the distal LSFA and popliteal stenoses and angioplasty of the multifocal stenoses of her anterior tibial artery down to the dorsalis pedis artery to restore reasonable flow to her foot that helped the ulcer heal.
Images in the top panel illustrate her disease before the interventions, those in the middle panel illustrate some intraprocedural steps (balloon angioplasty), while those in the bottom panel illustrate improved blood flow to the foot following treatment.



