When abscesses form deep in the pelvis and cannot be safely drained percutaneously through the anterior abdominal wall, they can be approached by inserting drainage catheters through the buttock (transgluteal), the vagina (transvaginal), or the rectum (transrectal). Often this is facilitated by the use of CT or ultrasound guidance depending on the approach chosen and the local availability of skills and technology.
In transgluteal drainage of pelvic collections the operator deploys a drainage catheter into the collection from the skin of the buttock through the greater or lesser sciatic foramen. The procedure can be risky, because there are important arteries, nerves, and veins in the area that can be hurt if care is not taken to avoid them; also planning for it may require intravenous administration of radiocontrast (intravenous dye) to distinguish these important structures.
The top-row images belong to a middle-aged woman with skin metastasis from small cell lung cancer who developed a deep pelvic abscess. The first image shows planning of transgluteal drainage of the collection, while the second image captures the final position of a 12F pigtail catheter deployed into it.


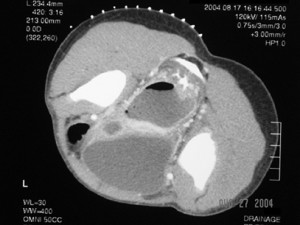
In the bottom row the first image illustrates the necessity of avoiding a frontal percutaneous approach to draining deep pelvic abscesses: this abscess is sandwiched between the rectum and the urinary bladder and in front of the bladder lies a loop of bowel and to its sides are the iliac vessels. The second image shows complete drainage of the abscess through the left buttock.